We identified differentiated thyroid cancer (dtc) survivors from seer registries and performed poisson regression to calculate the relative risks (rrs) of subsequent malignancies (sms) by different sites associated with radioactive iodine (rai) treatment, and the attributable risk proportion of rai for developing different sms. Current treatment including surgery (total thyroidectomy) followed by thyroid hormone therapy.
[ pmc free article ] [ pubmed ] [ google scholar ]
Thyroid cancer treatment radioactive iodine. It’s also used to treat thyroid cancer that spreads to other parts of your body. It is not a highly sought after diet but it is important to deprive the body of iodine. The thyroid gland gets iodine from certain foods and uses this to make essential thyroid hormones.
Learn more about radioiodine treatment, preparing for the procedure, and possible side effects. Radioactive iodine therapy is used in patients with an intermediate or higher risk of persistent or recurrent thyroid cancer. Rai kills these cells while leaving other body cells relatively unharmed.
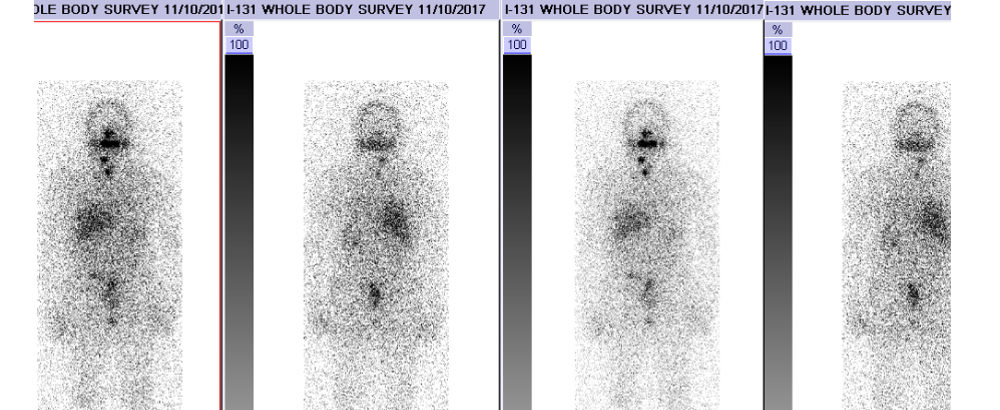
Radioactive iodine (rai) is also known as i131 and is a type of radioisotope treatment. Radioactive iodine treatment (rai) is a common way to treat differentiated forms of thyroid cancer ( papillary & follicular ). The thyroid gland is located within the vicinity of important structures in the neck, blood vessels, nerves and parathyroids glands.
This hormone is produced by the pituitary gland, which is located at the base of the brain and produces many hormones. Thyroid cancer is the fastest rising cancer in women. Most people with thyroid cancer get just one or two doses of rai therapy.
Radioactive iodine (rai) is a treatment that uses radiation to treat thyroid cancer. Radioactive iodine (rai) treatment is sometimes used after thyroidectomy for early stage cancers (t1 or t2), but the cure rate with surgery alone is excellent. We identified differentiated thyroid cancer (dtc) survivors from seer registries and performed poisson regression to calculate the relative risks (rrs) of subsequent malignancies (sms) by different sites associated with radioactive iodine (rai) treatment, and the attributable risk proportion of rai for developing different sms.
Radioisotopes are radioactive substances given in a pill that you swallow. If the cancer does come back, radioiodine treatment can still be given. Radioactive iodine treatment (rai) is usually recommended for patients who have been diagnosed with thyroid cancer and have recently had a total thyroidectomy to remove the cancer.
Radioactive iodine works as a “magic bullet” by getting taken up by. Radioactive iodine is a treatment for. That would include iodized salt, sea salt, any dairy, seafood, etc.
Tsh “tells” the thyroid to absorb iodine, which is then converted to thyroxine. What is radioactive iodine therapy? So, when a large dose of radioactive iodine is taken, the radiation collects in thyroid cells.
The study, led by researchers at the national cancer institute (nci), part of the national institutes of health, was. The impact of thyroid cancer and post‐surgical radioactive iodine treatment on the lives of thyroid cancer survivors: The patient will be admitted to a rai treatment room in hospital to undergo this treatment.
It’s effective because healthy cells in the body don’t usually absorb the radioactive iodine. Radioactive iodine therapy (rai) is used to destroy thyroid tissue cells in patients with grave�s disease and thyroid cancer. [ pmc free article ] [ pubmed ] [ google scholar ]
The radiation emitted by each of these forms of iodine can be detected from outside the patient to gain information about thyroid function and take pictures of the. It’s not the type of radiation you may think of when you think of cancer treatment. Iodine, in the form of iodide, is made into two radioactive forms of iodine that are commonly used in patients with thyroid diseases:
Recently, tyrosine kinase inhibitors (tkis) have shown activity in this disease. It is a useful treatment in thyroid cancer because the thyroid gland absorbs and stores most of the iodine in your body. Radioactive iodine therapy uses a form of iodine that sends out radiation to treat thyroid cancer.
You usually take radioactive iodine as a capsule that you swallow. Radioactive iodine treatment is a type of internal radiotherapy. Radioactive iodine can also be used to treat patients with nodular goiters that overproduce thyroid hormone in a similar fashion.
The treatment of differentiated thyroid cancer refractory to radioactive iodine (rai) had been hampered by few effective therapies. Current treatment including surgery (total thyroidectomy) followed by thyroid hormone therapy. Radioactive iodine (rai) treatment involves swallowing a capsule or liquid form of radioactive iodine that thyroid cells take up (absorb), destroying them.
You have the treatment as a drink or capsule which you swallow. Normal thyroid cells and thyroid cancer cells are unique because they are the only cells in. Radioactive iodine is usually given in pill form, but it can also be given in liquid form if needed.
This is typically done 6 to 8 weeks following surgery. If papilliary or follicular (but not medullary) cancer are diagnosed then the surgery will be followed by radioactive iodine (rai) treatment. This rai treatment is called thyroid ablation.
Before starting iodine radioactive treatment, doctors recommend to prepare the body by omitting food that may contain iodine. Although rai spreads through the body, it is mainly absorbed by thyroid cells or thyroid cancer cells. Radioactive iodine can be used for the treatment of overactive thyroid and certain types of thyroid cancer.
Treatment with radioactive iodine lowers your risk of your thyroid cancer coming back. Radioactive iodine treatment is frequently used to treat thyroid cancer. Patients who undergo a total thyroidectomy for thyroid cancer may benefit from a dose of radioactive iodine following the surgery.
Radioactive iodine (rai) can be used for the treatment of overactive thyroid (hyperthyroidism) and certain types of thyroid cancer.