You can get hpv from: Risk factors for hpv persistence and development of cervical cancer.

Cervical cancer is caused by sexually acquired infection with.
Risk of cervical cancer with hpv. To document the relationship between smoking and hpv infection, and the risk of developing preinvasive lesions and cervical carcinoma. Cervical cancer is the 14 th most common cancer in females in the uk. Estimates show that about 14 million new infections occur every year.
All people with a cervix are at risk for developing cervical cancer, although it develops most commonly in people over the age of 30. A total of 1,007 patients were recruited among women seen at the cervical pathology clinic of sant joan de déu university hospital in. Cervical cancer is caused by sexually acquired infection with.
Who is more likely to get cervical cancer. An individual is at increased risk of having hpv infection if he or she has had multiple sexual partners at any time or if he or she has a partner who has had multiple sexual partners. Human papillomavirus (hpv) causes almost all cases of cervical cancer, which is a common sexually transmitted infection.
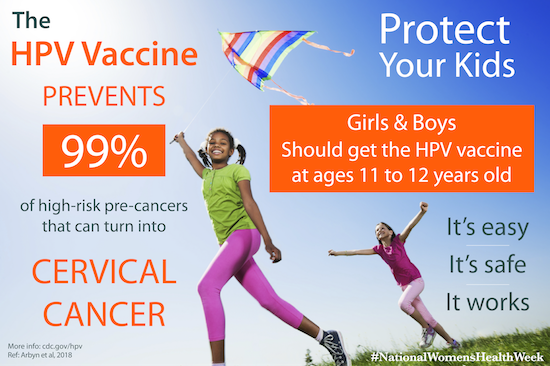
You can get hpv from: The number of sexual partners. Vaccines are available to prevent hpv.
These may eventually develop into cancer if they’re not found and removed in time. Vaginal, anal or oral sex; There are many types of hpv.
A persistent infection with oncogenic human papillomavirus (hpv) can lead to cervical precancerous lesions that may ultimately develop into cancer (crosbie et al., 2013). Hpv and 7 or more childbirths; Cervical scrapes from 116 british women referred with cervical cancer were tested for the presence of high oncogenic risk human papillomavirus (hpv) genotypes (hpvhr).
We aimed to assess how use of oral contraceptives affected risk of cervical cancer in women who tested positive for hpv dna. Hpv usually causes no symptoms so you can’t tell that you have it. Cervical cancer risk is almost three times higher in women who have had 6 or more sexual partners, compared with those who have had only one, a.
Use of oral contraceptives could increase risk of cervical cancer; The 3 hpv vaccines available in canada are gardasil, cervarix and gardasil 9. Vasive cervical cancer because of the long lead time (the time from hpv infection to the clinical detection of cervical cancer) and the low risk of.
Risk factors for hpv persistence and development of cervical cancer. Used birth control pills for 5. Human papilloma virus (hpv) is a major cause of cervical cancer practising safe sex can reduce the chances of hpv infection.
Hpv is so common that most people get it at some time in their lives. The median duration of new infections is 8 months. The two most important risk factors for cervical cancer are:
Other factors may be associated with cervical cancer risk because they increase the risk of human papillomavirus (hpv) exposure or persistent hpv infection (and/or may have direct effects, independent of hpv). There’s no approved hpv test to find hpv on the penis or vulva, or in the anus, mouth, or throat. Some hpv types can cause changes on a woman’s cervix that can lead to cervical cancer over time, while other types can cause genital or skin warts.
Cervical cancer affects the cervix, which connects the vagina to the uterus. There’s no test for men or women to check one’s overall “hpv status.” for cervical cancer screening, the american cancer. Screening for cervical cancer is an important part of routine health care for.
There are more than 100 identified hpv genotypes, and types 16 and 18 are the most common in cc (munoz et al., 2006 ). They can also cause anal cancer , penile cancer , vaginal cancer , vulvar cancer , and oropharyngeal cancer (cancer in the throat, usually the tonsils or the back of the tongue). The risk of acquiring hpv infection depends on:
Research shows that the risk of cervical cancer is higher among people who have: Acquiring infection with human papillomavirus (hpv), particularly types 16 and 18. However the effect of human papillomavirus (hpv), the main cause of cervical cancer, is not usually taken into account.
Smoking increases the risk of cervical cancer and makes it harder to treat abnormal cells in the cervix. Hpv vaccination and the risk of cervical cancer in this swedish registry study, quadrivalent human papillomavirus vaccination was associated with a. We sought to estimate the effect of hpv vaccination on cervical cancer incidence from observed data.
As reported in the lancet , the analysis found that vaccination at age 12 or 13 along with regular screening cut cervical cancer risk by almost 90% among women now in their 20s. Get vaccinated against human papillomavirus (hpv) hpv is a risk factor for developing squamous intraepithelial lesion (sil), which is a precancerous condition, and cervical cancer. Anyone with a cervix can get cervical cancer.
Cervical cancer develops in a woman�s cervix (the entrance to the uterus from the vagina). Cervical cancer cases plummeted among british women and girls who received a vaccination against the human papillomavirus (hpv), according to.