What genetic tests should lung cancer patients receive? Positiveselect ultimate is a genetic test that tests both cancer cells as well as normal blood cells.

A pilot study examining perceived benefits and barriers using health belief model.
Lung cancer genetic testing. Doctors use this type of testing to look for certain mutations. We know these changes as “biomarkers,” and doctors create a better approach to treatment for lung cancer by pinpointing them. When lung cancer is related to inherited genetic changes, the cancer risk follows an autosomal dominant pattern, which means one copy of the altered gene in each cell is sufficient to increase a person�s chance of developing the disease.
Your doctor should test your tumor for genetic mutations. The role of genetics and family history in the development of lung cancer is not well understood, according to dr. Genetics of lung cancer lung cancer is comprised of two main histologic subtypes:
Genetic testing involves looking for specific biomarkers , or changes in genes, that give the doctor more information about a. Harmful variants in some genes are known to be associated with an increased risk of developing cancer. The most common genetic changes that we test for in lung cancer are in the genes egfr, kras, and alk.
“since the discovery of the first gene linked to lung cancers in 2003, memorial sloan kettering has made the testing of genetic mutations in lung tumor specimens our mission,” says mark g. Can you explain what biomarker testing is? It is important to note that people inherit an increased risk of cancer, not the disease itself.
Biomarker testing is a genetic test to determine what mutations within the. Genetic testing plays an integral part in diagnosing and treating lung cancer. Steven kao (medical oncologist) features information on genetic testing including:
Evaluate the percentage of patients who had concurrent. Testing for gene mutations in lung cancer. Among the many benefits of targeted therapies is that they can block growth of cancer cells without harming healthy cells.
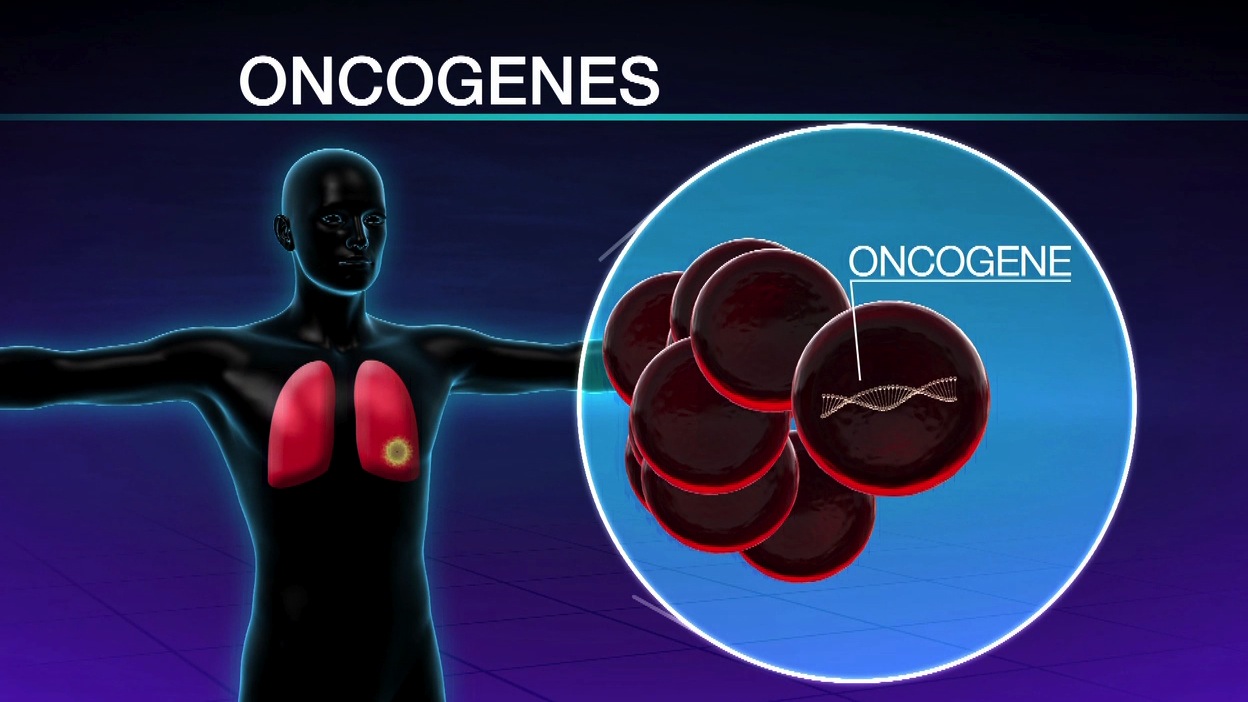
Megan baumgart, assistant professor of medicine, hematology/oncology at the wilmot cancer institute in rochester, but the risk appears to be highest for those with relatives diagnosed at a young age and those with multiple family. Subsets of nsclc may be characterized by recurrent driver mutations in multiple oncogenes like alk, braf, egfr, her2, met, kras, nras, and pik3ca among others 4. For further information or to engage with our lung cancer support nurse service you can.
Genetic testing for risk of lung cancer: Some lung cancers, such as non small cell lung cancer have changes in particular genes and proteins. How is genetic testing done?
What genetic tests should lung cancer patients receive? Positiveselect ultimate is a genetic test that tests both cancer cells as well as normal blood cells. Tumor normal match for lung cancer treatment options positiveselect ultimate.
The american lung association explains that, through genetic testing, doctors can identify what changes in lung cells trigger and contribute to cancer growth through genetic testing. One example of the benefit of getting your lung cancer genetic testing at holden is that we test for the kras g2c molecular target. What is genetic testing in lung cancer?
Assess the percentage of patients with a potentially targetable genetic alterations; A person with a specific mutation may benefit from a. Which mutations are relevant in lung cancer?
These changes can be used as targets for specific drug treatments. Kris, the william and joy ruane chair in. We also look at proteins on the tumor cells and stroma with immunohistochemistry.
When is genetic testing done? 2 arnold & marie schwartz college of. At md anderson, we look at a patient’s genetic sequencing, and the results from a fluorescence in situ hybridization test, commonly called fish.
Describe how targetable mutation genes interrelate with the genes identified as variants of unknown significance; Gene tests can also help your doctor find the right treatment for you if you do get lung cancer. Doctors may use genetic testing to diagnose and treat lung cancer.
In lung cancer, there is a little or no methylation of genes commonly methylated in other cancers, such as arf, cdkn2b, cttnb1, mlh1, and rb1. Genetic variants can have harmful, beneficial, neutral (no effect), or unknown or uncertain effects on the risk of developing diseases. Genetic testing for lung cancer can help narrow down the cause and determine the best method of treatment.
In addition to the positiveselect plus test benefits, positiveselect ultimate identifies somatic and. Learn more about lung cancer genetic testing. Genetic testing looks for specific inherited changes (variants) in a person’s genes.
Nsclc histology and the role of molecular testing. A pilot study examining perceived benefits and barriers using health belief model. They tell the cell which proteins to make.
Genes are found on chromosomes within all cells. These tests can identify specific genetic changes in the tumor cells that might be treatable with targeted therapies. Among the three main histologic subtypes of nsclc, lung adenocarcinoma (luad) is the most common, followed by lung squamous cell carcinoma (lusc) and large cell carcinoma ().besides having different histologic bases, these subtypes have disparate clinical presentations and unique genetic profiles ().
Furthermore, survival was increased for patients who were given drugs matched to specific driver mutations. Daniel saez, treatment and trials navigator at the go2 foundation for lung cancer, discusses biomarker testing and precision medicine in lung cancer. Karishma desai 1,, bupendra shah 2, hamid rahim 2, hongjun yin 3, john lonie 2.
This webinar, presented by dr. Genetic testing is playing a larger role in lung cancer care. The lung cancer epigenetic diagnostics may be based on the assessment of typical hypermethylated genes or the assessment of the hypermethylation of genes that are methylated in other cancers than lung cancer.
Knowing if you have lung cancer with a ret rearrangement is important no matter your stage of lung cancer but has the most treatment implications for stage four patients.